
What are the Different Stages of Bedsores?
At MedMalFirm.com, one of the most common questions our Houston bedsore attorney is asked is “what are the different stages of bedsores?” Many people don’t realize that there is more than one level of severity,…
At MedMalFirm.com, one of the most common questions our Houston bedsore attorney is asked is “what are the different stages of bedsores?” Many people don’t realize that there is more than one level of severity, or that bedsores can change over time.
Different Stages of Bedsores
Bedsores, also called pressure sores or decubitus ulcers, are injuries caused by unrelieved pressure or friction on the skin. Bedsores most commonly develop on parts of the body with bony prominences, such as the elbows, hips, shoulders, heels, or back.
These injuries range in severity from a mild discomfort to a deep open wound. There are four commonly recognized “stages” of bedsore, which the wounds based on the amount of damage.
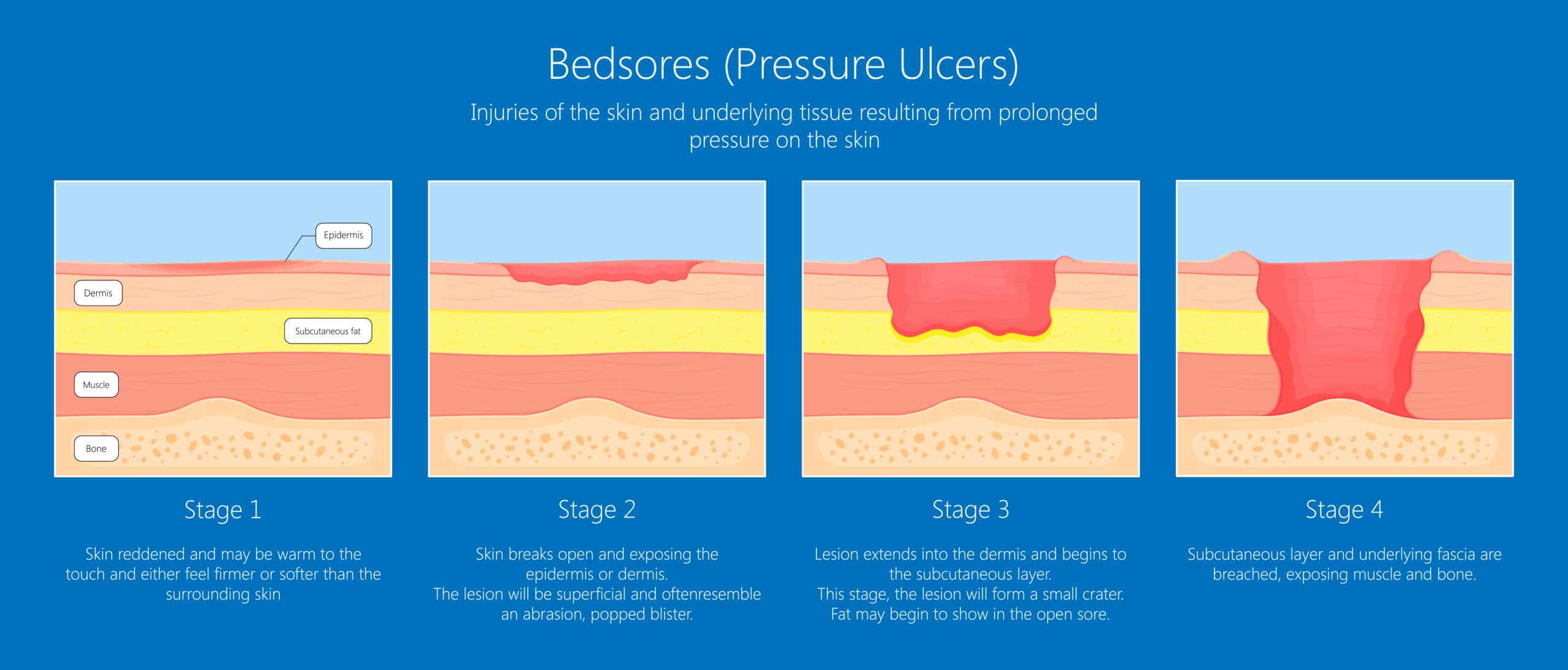
These stages are:
Stage 1
The least severe classification of bedsore is stage 1. Stage 1 is marked by symptoms including:
- Skin redness
- Warmth to the touch
- Swelling
With proper diagnosis and treatment, a stage 1 bedsore can resolve with minimal medical intervention. Therefore, most stage 1 cases have a recovery time of as little as three or four days. Without proper treatment, however, stage 1 bedsores will advance to stage 2 or worse.
Stage 2
A stage 2 bedsore is more severe than stage 1, but is generally considered treatable if diagnosed in a timely manner. At stage 2, the patient may experience:
- Loss of skin thickness around the wound
- An abrasion or blister
- Skin redness
- Warmth to the touch
By stage 2, the bedsore is developed and it is important to initiate treatment and relieve pressure. With proper medical care, stage 2 bedsores can resolve in as little as one week, or may take up to three weeks. In contrast, without proper care, stage 2 bedsores will advance to stage 3.
Stage 3
A stage 3 bedsore is certainly a serious wound that requires immediate medical care. By stage 3, the patient may be experiencing severe pain as well as:
- Full skin thickness loss (fatty tissue may be visible in the open wound)
- Necrosis
- Extreme skin redness
- Skin hardening
- Pus or drainage
- Foul odor
Stage 3 bedsores require immediate medical intervention. The risk of infection is high due to the open wound and decaying tissues. Infection often leads to sepsis, as well. With proper treatment, stage 3 bedsores can resolve, though recovery time is between one to four months.
Stage 4
Stage 4 bedsores are the most severe that are classified. At this stage, there is almost always a deep open wound. These sores are very difficult to treat, and can certainly lead to a series of complications. At stage 4, the patient may experience:
- Necrosis
- Damage to muscle or bone
- A deep crater exposing tissue and bone
- Significant pus or drainage
- Foul odor
- Purple or black skin discoloration
Stage 4 bedsores require medical care from a specialized wound care team because they are extensive. These wounds often require surgery to remove dead tissue and repair any damaged structures. Stage 4 wounds are very vulnerable to bacteria and viruses, so infection control is important. With proper treatment, a stage 4 bedsore can resolve in two to six months.
Can All Bedsores be Staged?
If a bedsore develops to a point where staging is impossible, it may be classified as “Unstageable”. That means that the doctor cannot identify the stage by visual examination. Unstageable bedsores are often so advanced that the wound is life-threatening.
There is also a classification called a “suspected deep tissue injury (SDTI). These bedsores are apparent on visual examination, but can be deceiving. With an SDTI, the wound appears to be a stage 1 or 2 on the surface, but there is more extensive underlying damage suspected, but the wound has not opened up.
Who is Vulnerable to Develop a Bedsore?
The individuals most vulnerable to developing a bedsore are those with limited mobility. This includes:
- Patients who are hospitalized
- Individuals with limited mobility while recovering from an injury
- Individuals who are wheelchair bound
- Nursing home residents
Anyone in these situations should certainly be careful to monitor their skin health. Keeping skin clean, dry, and moisturized is a first line of defense against bedsores. Further, caregivers should be careful to make sure that these individuals get help to reposition themselves or move around. This prevents friction and pressure from building up on bony parts of the body.
Can Bedsores be Prevented?
Bedsores are considered preventable in almost every case. They are also considered to be one of the most common preventable complications experienced by hospital patients. This certainly begs the question of why they occur at all if they can be prevented? After all, we know who is vulnerable and why.
In 2016, The Joint Commission published a report recommending the following strategies for preventing bedsores:
- Risk Assessment – Patients with limited mobility should be assessed for a risk of developing a bedsore. This includes considerations for conditions like diabetes, previous bedsores, or vascular problems.
- Skin Care – Patients should be assisted in maintaining good skin care habits, including proper washing, drying, moisturizing, and assessing possible injuries.
- Nutrition – Lack of proper nutrition increases the risk of developing bedsores.
- Positioning – The standards of care for immobile patients requires they be repositioned at least every two hours to prevent pressure buildup.
There are clear guidelines for healthcare providers and caregivers for preventing bedsores. Likewise, there are standards for managing wounds that develop. Unfortunately, many hospitals, nursing homes, and caregivers do not follow these guidelines. As a result, patients are left at risk of developing painful and even life-threatening injuries.
Have Questions or Concerns about Bedsores?
If you or a loved one have developed a bedsore while in a hospital or nursing home, contact MedMalFirm.com. Our Houston bedsore attorney can help you determine if your bedsore is a result of healthcare negligence.
